Hospitals bracing for virus outbreak
Workers on practice runs; isolation wards readied
By Catherine Ho
As the new coronavirus continues to spread in Europe, the Middle East and Asia — and Solano County recorded the first U.S. case unrelated to international travel, raising fears of a local outbreak — Bay Area hospitals are bracing for the possibility of large numbers of coronavirus patients at a time many are already stretched thin because of the flu season.
Hospitals are doing practice runs for workers on how to triage and treat coronavirus patients, including putting on and taking off protective gowns, gloves and glasses, and are considering plans to potentially add isolation rooms or isolation wards if the need arises.
Many of these infectious disease protocols were established after the last global pandemic — the 2009 H1N1 influenza that killed at least 152,000 people worldwide, including 12,000 in the U.S. — and are similar to the way hospitals treat patients with highly infectious airborne diseases like tuberculosis and measles.
“We have done drills and simulations to be ready for COVID-19,” said Dr. Stephen Parodi, an infectious disease physician at Kaiser Permanente’s Solano County medical centers. “Certainly the emergency departments have received quite a bit of training and simulation. ... And we’ve also done training for medical and surgical staff — individuals who work in a regular medical ward and have received training as well.”
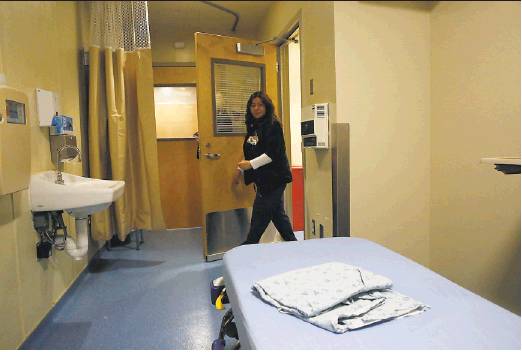
That includes isolating patients in what’s called “negative pressure rooms,” which have a separate air circulation system from the rest of the hospital. These rooms have HVAC systems that suck in contaminated air, filter it, and release it outside so that it doesn’t contaminate the air in the rest of the hospital.
Every hospital is required to have negative pressure rooms, though the number at each hospital varies depending on the level of risk for infectious diseases in their region. The San Francisco Department of Public Health said there are more than 100 at hospitals in the city.
Northern California hospitals have collectively admitted at least 17 people who have tested positive for coronavirus, most of them passengers from the cruise ship Diamond Princess, and are said to be deploying these practices already — though county health officials have declined to name most of the hospitals.
If the number of coronavirus patients were to grow into the dozens or even hundreds — as is the case in Italy, South Korea and Iran — hospitals cannot add negative pressure rooms because they are constructed when the hospital is built. But they can add isolation rooms, which are less stringent than negative pressure rooms and are used for people with viruses that are spread by droplets, such as the flu, as opposed to viruses that are airborne, such as measles and TB. Droplets are spread 3 to 6 feet if someone sneezes or coughs, then settle onto the floor and are not as transmissible as when a virus is airborne, when contamination stays in the air for much longer.
It appears the new coronavirus is likely spread by droplets, and is not airborne. So if a large number of cases were to appear in the U.S., hospitals could potentially do droplet isolation protocols instead of airborne protocols.
“It gives us more options if it’s a droplet-spread disease, in the types of rooms to allow us to safely isolate an individual,” Parodi said.
Hospital administrators are in constant conversations with state health officials to monitor supplies that would be needed in the event of an outbreak, such as masks, protective gowns and glasses. Hospital systems and public health departments maintain a regional stockpile of such items so they can be shared with other nearby hospitals if they need it, said Dr. Kathleen Jordan, an infectious disease specialist and chief medical officer at Dignity Health’s St. Francis Memorial Hospital in San Francisco.
“We have not tried to order and not been able to get any at this time,” she said. “We’ve been able to fill our current demand.”
There have been 60 confirmed cases of coronavirus in the U.S., including 28 in California (mostly cruise ship passengers), and they have either self-isolated at home or been hospitalized after testing positive while under quarantine at Travis Air Force Base in Fairfield. On Wednesday evening, the CDC confirmed one Solano County resident tested positive for the virus but had not traveled recently to countries where coronavirus is spreading, or had any known contact with anyone with a confirmed case of coronavirus. This suggests the virus may be spreading in the community.
If the number of U.S. cases increases, “most of the protocols should be pretty reasonable, but what we really need to be wary of is the volume,” said Dr. Yvonne Maldonado, an infectious disease specialist at Stanford Medicine. “How many people do we think are going to come in?
“What we think may happen is the vast majority of people won’t be very sick, but even if the proportion isn’t high of severe illness, even a small number of people coming in ... could overwhelm a hospital’s facilities,” she said. “If you need to isolate people, we don’t have a lot of isolation rooms. We all deal with how to figure those plans out.”
Hospitals can and have moved quickly to accommodate large numbers of unexpected patients. When an Asiana Airlines flight crashed at SFO in 2013, for instance, Stanford Hospital got about 55 patients and improvised space to treat them.
“That wasn’t a viral infection, but there were a lot trauma patients,” Maldonado said. “You have to figure out where to put everyone. You tailor your needs to what you know you have available. ... You can decide to put everyone we know that has a particular symptom in one ward, if that ward is bigger. ... You can turn wards into isolation wards if you have a lot of patients.”
Maldonado said the hospital has not made any of those types of decisions yet with the new coronavirus, but if the number of cases grows, hospital administrators would start discussing with their engineers which rooms would have the best air flow to prevent contamination from going into other areas of the hospital.
“It’s hypothetical because we don’t have an outbreak,” she said.
A more pressing problem, she said, is that many hospitals have yet to receive lab test kits from the CDC that would allow for faster test results to confirm whether someone has coronavirus. The CDC sent out test kits earlier this month so state and local labs could help relieve the CDC backlog, but some of the tests turned out to be flawed and replacement tests have not been distributed.
“The biggest question is when are we going to get the test kits?” Maldonado said. “Without those, we don’t know who has a respiratory virus versus who has coronavirus because you don’t want to put people in the same unit. ... Test kits would be really helpful for us to be able to run those tests in a couple hours and know, ‘This is the flu versus COVID,’ and if it’s the flu it’s a little easier for us to deal with. We really want that kit. It’s just been taking such a long time to get the kit.”
It might not be hospitals alone that end up housing large numbers of coronavirus patients, most of whom are likely to be asymptomatic or show mild to moderate symptoms that don’t require hospitalization. State health officials are seeking sites to potentially house cruise ship passengers currently being held at Travis Air Force Base — including one potential stateowned facility in Costa Mesa (Orange County), Fairview Developmental Center. The plan was met with resistance from Costa Mesa officials who say they were not properly consulted and fear that it might put local residents at risk for infection. Costa Mesa sued the state in an attempt to prevent the potential transfer of the patients, and a federal judge on Monday agreed to halt the transfer, at least until next week.
Parodi of Kaiser said the more widespread availability of telemedicine today, compared with its more limited use a decade ago during the H1N1 pandemic, may prove helpful in containing the coronavirus.
“You can video chat, text with medical providers, and not necessarily have to go to see your doctor,” he said. “The ability to evaluate somebody or even get medication if that’s needed to a person via virtual means is something that we’re actively discussing in our preparation.”
Catherine Ho is a San Francisco Chronicle staff writer. Email: cho@sfchronicle.com Twitter: @Cat_Ho