Why some doctors won’t break bad news
By JoNel Aleccia KAISER HEALTH NEWS
PORTLAND, Ore. — After nearly 40 years as an internist, Dr. Ron Naito knew what the sky-high results of his blood test meant. And it wasn’t good.
But when he turned to his doctors last summer to confirm the dire diagnosis — stage 4 pancreatic cancer — he learned the news in a way no patient should.
The first physician, a specialist Naito had known for 10 years, refused to acknowledge the results of the “off-the-scale” blood test that showed unmistakable signs of advanced cancer.
“He simply didn’t want to tell me,” Naito said.
A second specialist performed a tumor biopsy, and then discussed the results with a medical student outside the open door of the exam room where Naito waited.
“They walk by one time and I can hear (the doctor) say ‘5 centimeters,’ ” Naito said. “Then they walk the other way and I can hear him say, ‘Very bad.’ ”
Months later, the shock remained fresh.
“I knew what it was,” Naito said last month, his voice thick with emotion. “Once (tumors grow) beyond 3 centimeters, they’re big. It’s a negative sign.”
The botched delivery of his grim diagnosis left Naito determined to share one final lesson with future physicians: Be careful how you tell patients they’re dying.
Since August, when he calculated he had six months to live, Naito has mentored medical students at Oregon Health & Science University and spoken publicly about the need for doctors to improve the way they break bad news.
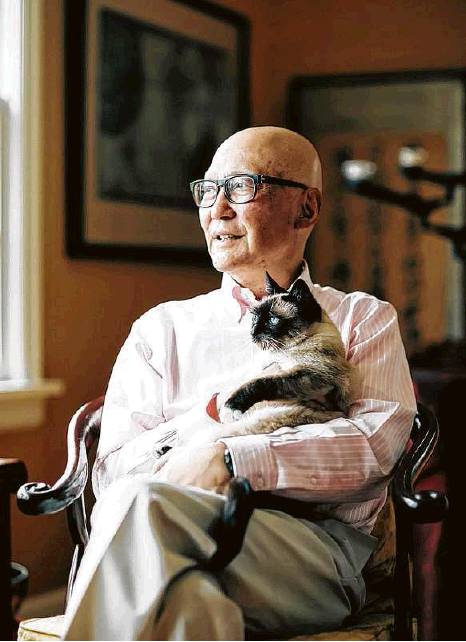
“Historically, it’s something we’ve never been taught,” said Naito, thin and bald from the effects of repeated rounds of chemotherapy. “Everyone feels uncomfortable doing it. It’s avery difficult thing.”
Robust research shows doctors are notoriously bad at delivering life-altering news, said Dr. Anthony Back, an oncologist and palliative care expert at the University of Washington in Seattle, who wasn’t surprised that Naito’s diagnosis was poorly handled.
“Dr. Naito was given the news in the way that many people receive it,” said Back, who is a co-founder of VitalTalk, one of several organizations that teach doctors to improve their communication skills. “If the system doesn’t work for him, who’s it going to work for?”
Up to three-quarters of all patients with serious illness receive news in what researchers call a “suboptimal way,” Back estimated.
“ ‘Suboptimal’ is the term that is least offensive to practicing doctors,” he added.
Too often, doctors avoid such conversations entirely, or they speak to patients using medical jargon. They frequently fail to notice that patients aren’t following the conversation or that they’re too overwhelmed with emotion to absorb the information, Back noted in a recent article.
That’s because for many doctors, especially those who treat cancer and other challenging diseases, “death is viewed as afailure,” said Dr. Brad Stuart, a palliative care expert and chief medical officer for the Coalition to Transform Advanced Care, or C-TAC.
They’ll often continue to prescribe treatment, even if it’s futile, Stuart said. It’s the difference between curing a disease and healing a person physically, emotionally and spiritually, he added.
“Curing is what it’s all about, and healing has been forgotten,” Stuart said.
The result is that dying patients are often ill-informed. A 2016 study found that 5 percent of cancer patients accurately understood their prognoses well enough to make informed decisions about their care. Another study found that 80 percent of patients with metastatic colon cancer thought they could be cured. In reality, chemotherapy can prolong life by weeks or months, and help ease symptoms, but it will not stop the disease.
The doctors who treated him had the best intentions, said Naito, who declined to publicly identify them or the clinic where they worked. Reached for verification, clinic officials refused to comment, citing privacy rules.
Indeed, most doctors consider open communication about death vital, research shows. A 2018 telephone survey of physicians found that nearly all thought end-of-life discussions were important — but fewer than a third said they had been trained to have them.
Back, who has been urging better medical communication for two decades, said there’s evidence that skills can be taught — and that doctors can improve. Many doctors bridle at any criticism of their bedside manner, viewing it as something akin to “character assassination,” Back said.
“But these are skills, doctors can acquire them, you can measure what they acquire,” he said.
For instance, doctors can learn — and practice — a simple communication model dubbed “Ask-Tell-Ask.” They ask the patient about their understanding of their disease or condition; tell him or her in straightforward, simple language about the bad news or treatment options; then ask if the patient understood what was just said.
Naito shared his experience with medical students in an OHSU course called “Living With Life-Threatening Illness,” which pairs students with ill and dying patients.
“He was able to talk very openly and quite calmly about his own experience,” said Amanda Ashley, associate director of OHSU’s Center for Ethics in Health Care. “He was able to do a lot of teaching about how it might have been different.”
Naito, who has endured 10 rounds of chemotherapy, recently granted the center $1 million from the foundation formed in his name. He said he hopes future doctors and current colleagues will use his experience to shape the way they deliver bad news.
“The more people know this, it doesn’t have to be something you dread,” he said. “I think we should remove that from medicine. It can be a really heartfelt, deep experience to tell someone this, to tell another human being.”
“Historically, it’s something we’ve never been taught. Everyone feels uncomfortable doing it. It’s a very difficult thing.”
Dr. Ron Naito, on telling patients they’re dying